- Get link
- X
- Other Apps
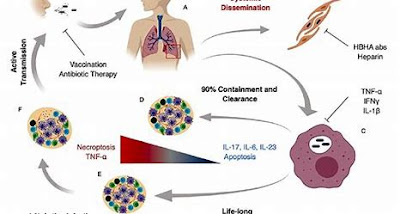
Mycobacterium tuberculosis is a bacterium that causes tuberculosis (TB), a serious infectious disease that primarily affects the lungs but can also affect other parts of the body. TB is a global health concern and is one of the top infectious disease killers worldwide. Public health measures, including contact tracing and isolation of active TB cases, also play a crucial role in preventing the spread of the disease.
- Classification
- It is an acid-fast, rod-shaped bacterium.
- Kingdom:- Monera
- Domain:- Bacteria
- Phylum:- Actinomycetota
- Class:- Actinomycetia
- Subclass:- Actinobacteridae
- Order:- Actinomycetales
- Suborder:- Corynebacterineae
- Family:- Mycobacteriaceae
- Genus:- Mycobacterium
- Species:- tuberculosis
- Epidemiology:-
- TB is a global health challenge, with a disproportionate burden in low- and middle-income countries.
- It's estimated that over 10 million people worldwide develop active TB each year, and approximately 1.4 million people die from the disease annually.
- Vulnerable populations such as those with weakened immune systems (e.g., due to HIV infection), people living in crowded and unsanitary conditions, and individuals with limited access to healthcare are at higher risk.
- Tuberculosis in History:-
- TB has a long history, and historical figures such as Frederic Chopin, George Orwell, and John Keats are believed to have suffered from the disease.
- In the past, TB was often referred to as
"consumption" due to the characteristic wasting away of the body seen
in advanced cases.
- Disease Presentation
- TB can manifest in two forms: latent TB infection and active TB disease.
- Transmission:-
- TB is primarily transmitted from person to person through the air when an infected individual coughs, sneezes, or talks.
- People
in close contact with someone who has active TB are at the highest risk of
contracting the disease.
- Tuberculosis Stages:-
- Exposure:-
- This is the initial stage when a person inhales M. tuberculosis bacteria from an infected individual.
- Most people do not develop active TB disease at this stage, and the immune system can control the infection, leading to latent TB infection.
- Latent TB Infection (LTBI):-
- In LTBI, bacteria are present in the body but are inactive.
- There are no symptoms, and the person is not contagious.
- However, LTBI can progress to active TB disease if the immune system weakens.
- Active TB Disease:-
- When the bacteria become active and multiply, causing symptoms, it's called active TB disease.
- Symptoms can vary but often include a
persistent cough, fever, night sweats, and weight loss.
- Airborne Transmission:-
- TB is primarily spread through the air via droplets expelled when an infectious person coughs, sneezes, or talks.
- Good ventilation and respiratory hygiene are critical in healthcare settings and households with TB cases.
- Extra-Pulmonary TB:-
- While TB primarily affects the lungs, it can also infect other parts of the body, leading to extra-pulmonary TB.
- Common sites include the lymph nodes, bones, joints, and the central nervous system (meningitis).
- Diagnosis and treatment may differ for extra-pulmonary TB
compared to pulmonary TB.
- Directly Observed Therapy (DOT):-
- DOT is a strategy used to ensure that individuals with active TB take their medications regularly and complete their treatment.
- Healthcare workers or trained volunteers directly observe the patient taking each dose of medication to improve adherence and reduce the risk of drug resistance.
- TB and Gender:-
- TB affects men and women differently, with different social and biological factors influencing risk and outcomes.
- Gender-sensitive approaches are important in TB care and prevention.
- Tuberculosis and Mental Health:-
- TB can have psychological and social impacts on patients, including stigma and discrimination.
- TB programs often incorporate mental health support to address these issues and improve treatment adherence.
- TB and the Immune System:-
- The body's immune response plays a crucial role in controlling TB infection.
- Immunocompromised individuals, such as those with
HIV, are more susceptible to TB, and TB can worsen the course of HIV infection.
- TB and Stigma:-
- TB has historically been associated with stigma and discrimination, which can hinder efforts to control the disease.
- Raising awareness and reducing stigma are critical aspects of TB advocacy.
- Active Case Finding:-
- In some settings, active case-finding strategies involve actively searching for TB cases in high-risk populations, such as mining communities, prisons, and healthcare facilities, to diagnose and treat cases early.
- TB in the Era of COVID-19:-
- The COVID-19 pandemic has had an impact on TB diagnosis, treatment, and control efforts.
- Disruptions in healthcare services and increased vulnerability among certain populations have raised concerns about TB resurgence.
- Diagnosis
- TB can be diagnosed through various methods, including the tuberculin skin test (TST), interferon-gamma release assays (IGRAs), and various imaging and laboratory tests.
- Definitive diagnosis often involves culturing the bacteria from a sputum sample.
- In addition to traditional methods, newer diagnostic tools like molecular assays (e.g., Xpert MTB/RIF), interferon-gamma release assays (IGRAs), and radiographic imaging (e.g., chest X-rays and CT scans) are valuable for diagnosing TB.
- Molecular Epidemiology:-
- Molecular techniques like DNA fingerprinting (using methods such as IS6110 restriction fragment length polymorphism) help trace the transmission of specific strains of M. tuberculosis.
- This is important for
identifying TB outbreaks and patterns of transmission.
- Latent TB Testing:-
- There are two common tests to detect latent TB infection:
- Tuberculin Skin Test (TST or Mantoux test):-
- A small amount of tuberculin protein is injected under the skin, and a delayed skin reaction is assessed.
- Interferon-Gamma Release Assays (IGRAs):-
- These blood tests measure the immune response to specific TB antigens.
- Contact Tracing:-
- When an active TB case is identified, public health authorities often conduct contact tracing to locate and test individuals who may have been exposed to the bacterium.
- This helps identify latent infections and prevent further transmission.
- GeneXpert:-
- The GeneXpert MTB/RIF assay is a molecular diagnostic test that rapidly detects the presence of M. tuberculosis and assesses its resistance to rifampin.
- It has greatly improved TB diagnosis, especially in settings with limited laboratory infrastructure. "
- For more detail GeneXpert " (gyaan.site)
- HIV Co-infection:-
- HIV infection is a significant risk factor for developing active TB, as it weakens the immune system.
- TB is one of the leading causes of death among people with HIV/AIDS.
- Screening and treatment for TB are essential components of HIV care and treatment programs.
- Mycobacterium tuberculosis Management
- This bacteria can be manage by various ways:
- Treatment:-
- TB is treatable with a combination of antibiotics, typically over a period of six to nine months.
- The most used antibiotics include isoniazid, rifampin, ethambutol, and pyrazinamide.
- Compliance with the full course of treatment is crucial to prevent drug resistance.
- Drug Resistance:-
- Mycobacterium tuberculosis can develop resistance to the antibiotics used to treat TB.
- Drug-resistant TB strains are a significant concern, as they require more extended and more complex treatment regimens.
- BCG Vaccine:-
- The Bacilli Calmette-Guérin (BCG) vaccine is used in many countries to prevent severe forms of TB, particularly in children.
- However, it provides varying levels of protection and is less effective against
adult pulmonary TB. BCG vaccination policies vary by country.
- Multi-Drug Resistant TB (MDR-TB) and Extensively Drug-Resistant TB (XDR-TB):-
- TB drug resistance is a serious concern. MDR-TB is resistant to at least two of the most potent first-line drugs, isoniazid, and rifampin.
- XDR-TB is a more severe form, resistant not only to first-line drugs but also to some second-line drugs, making treatment much more challenging and less effective.
- Prevention:-
- TB prevention strategies include vaccination with the Bacilli Calmette-Guérin (BCG) vaccine, which can help protect against severe forms of TB in children.
- Additionally, identifying and treating latent TB infections in high-risk populations is a preventive measure.
- Nutrition and TB:-
- Proper nutrition is crucial for TB patients.
- Malnutrition weakens the immune system, making individuals more susceptible to TB and hindering recovery.
- Adequate nutrition is considered an essential
component of TB treatment and care.
- Quarantine and Isolation:-
- In cases of active TB disease, patients are often isolated to prevent the spread of the bacteria to others.
- Quarantine measures may also be applied to individuals with latent TB who are at risk of developing active disease.
- Isoniazid Preventive Therapy (IPT):-
- IPT involves giving isoniazid (an anti-TB drug) to individuals with latent TB infection to prevent the development of active TB disease.
- It's particularly beneficial for people at high risk of progressing to active TB.
- Community Health Workers:-
- Trained community health workers often play a crucial role in TB control efforts, particularly in underserved and resource-limited settings.
- They help with case finding, treatment adherence support, and patient education.
- Healthcare workers who care for TB patients are at increased risk of infection.
- Infection control measures, including proper use of personal protective equipment and healthcare worker education, are essential to reduce this risk.
- Mycobacterium tuberculosis Complex
- Besides M. tuberculosis, the Mycobacterium tuberculosis complex includes several other closely related species.
- These include M. bovis (affecting cattle but can infect humans through contaminated dairy products), M. africanum (found primarily in West Africa), and M. microti (associated with tuberculosis in some animals).
- Zoonotic TB:-
- M. bovis, a member of the M. tuberculosis complex, can be transmitted to humans through consumption of unpasteurized dairy products or close contact with infected animals.
- This is known as zoonotic TB and is a concern in some agricultural and pastoralist communities.
- Besides M. bovis, other mycobacteria can infect animals and cause tuberculosis-like diseases in various species.
- This can have implications for veterinary and public health.
- Global Impact
- TB remains a major global health issue, particularly in regions with limited access to healthcare and resources.
- Efforts to control and eliminate TB include improved diagnostics, access to treatment, and public health interventions.
- Global Efforts:-
- Organizations like the World Health Organization (WHO) and the Stop TB Partnership work tirelessly to reduce the global burden of TB through initiatives like the "End TB Strategy."
- These efforts aim to diagnose and treat TB cases, prevent transmission, and ultimately eliminate the disease as a public health threat.
- Tuberculosis in Prisons:-
- Prisons can be high-risk environments for TB transmission due to overcrowding and limited access to healthcare.
- Tuberculosis control programs often target correctional facilities to diagnose, treat, and prevent the spread of the disease among inmates and staff.
- TB and Vulnerable Populations:-
- Homeless individuals, refugees, migrants, and those
with substance use disorders are at higher risk for TB due to various factors,
including limited access to healthcare, crowded living conditions, and social
determinants of health.
- Pediatric TB:-
- TB can affect children, and pediatric TB often presents differently than in adults.
- Diagnosis and treatment in children may require specialized approaches and medications.
- Pediatric TB can be challenging to diagnose and treat.
- Specialized formulations of anti-TB drugs are available for children, and management often involves close collaboration between pediatricians and TB experts.
- TB in High-Burden Countries:-
- Countries with a high burden of TB often have National TB Programs (NTPs) supported by international agencies like the WHO, the Global Fund to Fight AIDS, Tuberculosis and Malaria, and non-governmental organizations to improve TB control efforts.
- Global Partnerships:-
- TB control is a global effort involving partnerships between governments, international organizations, civil society, and the private sector.
- These collaborations are crucial for achieving TB control and elimination goals.
- TB Elimination Goals:-
- Several countries and organizations have set ambitious goals to eliminate TB as a public health problem.
- These goals often involve reducing TB incidence and mortality rates by a specified percentage by a target year.
- Achieving these goals requires sustained efforts in prevention, diagnosis, and treatment.
- Global TB Report:-
- The World Health Organization (WHO) publishes an annual
Global Tuberculosis Report, providing comprehensive data and analysis on the
global TB situation, including case numbers, treatment outcomes, and funding
gaps.
- The Global Plan to End TB:-
- The Global Plan to End TB is a roadmap set forth by the Stop TB Partnership to accelerate efforts to eliminate TB.
- It outlines strategies to reduce TB incidence, mortality, and catastrophic costs for affected families.
- TB and Social Determinants of Health:-
- TB incidence is often linked to social determinants of health, including poverty, malnutrition, overcrowded living conditions, and limited access to healthcare.
- Addressing these underlying factors is crucial in TB prevention and control.
- Research and Development
- Ongoing research aims to develop better diagnostic tools, more effective treatments, and a vaccine with higher efficacy against TB.
- The development of a highly effective TB vaccine remains a major priority in the fight against TB.
- TB and Antibiotic Resistance:-
- The development of new antibiotics and treatment regimens is critical to combating drug-resistant TB.
- Research continues to
focus on finding novel therapies and approaches to tackle this challenging
issue.













Comments
Post a Comment